What are the common injuries associated with motor vehicle accident?
Neck or back injury caused by whiplash is the most common injury among car occupants. This can lead to chronic whiplash-associated disorder.
Other injuries include head, thoracic, abdominal, pelvic or limb injury.
What is Whiplash Associated Disorder?
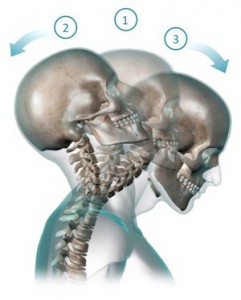
Whiplash is a collective term applied to injuries of the spine that often result from an automobile accident, usually when a vehicle has been hit from rear. Whiplash associated disorder (WAD) describes injury sequelae and symptoms. The condition occurs when sudden acceleration-deceleration forces the spine to whip back and forth (hyper-extension followed by hyper-flexion).
Common Symptoms
Pain & stiffness of the neck or back
Referred pain to shoulder or hips
Numbness & weakness of arms or legs
Headaches at the base of skull
When should you consult a doctor after a motor vehicle accident?
You should consult a doctor if:
- It becomes painful to move your head
- The pain spreads to your shoulder, hips, arms or legs
- You experience numbness, tingling or weakness in your arms or legs
What motor vehicle injuries does Dr. Banionis treat?
Neck Pain
Shoulder pain
Rotator cuff injury
Elbow or wrist pain
Back Pain
Herniated disc
Facet dysfunction
Sciatica
What are the treatment options available for patients suffering from motor vehicle injuries?
The goal of our treatment is functional rehabilitation. While eliminating chronic back or neck pain is extremely hard, our functional rehabilitation program seeks to return patients to levels of activity that they were able to perform prior to suffering from back or neck pain. We have a multi-modal approach to treatment, where we use many different approaches to treat pain.
Our multi-modal approach includes:
Muscle strengthening regimen
We encourage our patients to begin stretching exercises and resume normal daily activities as soon as possible, while avoiding movements that aggravate pain. Strengthening exercises, beyond general daily activities, are not advised for acute low back pain, but may be an effective way to speed recovery from chronic or subacute low back pain. Physical therapy programs to strengthen core muscle groups that support the low back, improve mobility and flexibility, and promote proper positioning and posture are often used in combinations with other interventions.
Medications
The following are the main types of medications used for low back pain:
Analgesic medications are those specifically designed to relieve pain. They include over-the-counter acetaminophen and aspirin, as well as prescription opioids such as codeine, oxycodone, hydrocodone, and morphine. Opioids should be used only for a short period of time and under a physician’s supervision. People can develop a tolerance to opioids and require increasingly higher dosages to achieve the same effect. Opioids can also be addictive. Their side effects can include drowsiness, constipation, decreased reaction time, and impaired judgment. The use of opioids is heavily regulated by Drug Enforcement Agency (DEA). In our practice all patients who are being treated with opioids are required to sign an Opioid Agreement and periodically undergo urine and blood testing.
Anticonvulsants—drugs primarily used to treat seizures—may be useful in treating people with radiculopathy and radicular pain.
Antidepressants such as tricyclics and serotonin and norepinephrine reuptake inhibitors have been commonly prescribed for chronic low back pain, but their benefit for nonspecific low back pain is unproven, according to a review of studies assessing their benefit.
Counter-irritants such as creams or sprays applied topically stimulate the nerves in the skin to provide feelings of warmth or cold in order to dull the sensation of pain. Topical analgesics reduce inflammation and stimulate blood flow.
Minimally Invasive Treatment
Nerve block therapies aim to relieve chronic pain by blocking nerve conduction from specific areas of the body. Nerve block approaches range from injections of local anesthetics, botulinum toxin, or steroids into affected soft tissues or joints to more complex nerve root blocks and spinal cord stimulation. The success of a nerve block approach depends on the ability of a practitioner to locate and inject precisely the correct nerve. Some of the common treatment options include:
Epidural space is a potential space within the spinal canal. It surrounds the outermost covering of the spinal cord (dura mater). It contains nerve roots, blood vessels & fatty tissue. A relatively small amounts of corticosteroids together with a local anesthetic are injected into the epidural space around the spinal cord and spinal nerves. The anti-inflammatory effects of the corticosteroid is responsible for providing pain relief. Epidural Steroid Injections help patients suffering from disc herniation, disc bulges, degenartive disc disease, sciatica & spinal stenosis. It is considered to be an integral part of nonsurgical management of radicular pain from spinal disorders.
Facet Joint Injection or Medial Branch Block
The facet joints are formed by the superior and inferior articular processes of each vertebra. Every vertebrae in the spine has a left and right facet joint. Each joint gets its sensation from a tiny nerve called Medial Branch. These joints also allow the spine to bend and twist, and they keep the back from slipping too far forward or twisting without limits. Breakdown or degeneration of these joints can lead to pain in the back, arms or legs leading to a diagnosis of facet joint disease. For treatment of Facet Joint Disease, we initially perform Facet Joint Injection or Medial Branch Block with a local anesthetic or numbing medicine. This injection helps us identify the site of back or neck pain. This is usually followed by Radiofrequency Ablation (RFA).
Radiofrequency ablation is a procedure in which radiofrequency waves are used to produce heat on specifically identified nerves. Prior to Radiofrequency Ablation, the nerves to be ablated are identified through Facet Joint Injection or Medial Branch block. By generating heat around the nerve, the ability of the nerve to transmit pain signals to the brain is destroyed, thus ablating the nerve. Patients with back, neck or leg pain can get pain relief from these procedures. Pain relief can last anywhere from six months to two years.
Our blood contains several types of cells such as red blood cells (RBCs), white blood cells (WBCs) and platelets. Platelets contain a number of growth factors, cytokines, proteins and other bioactive factors that initiate and regulate wound healing. Platelet rich plasma therapy uses patient’s own blood components to stimulate a healing response in damaged tissues. Depending on extent of injury, will depend on amount of blood that is drawn and centrifuged with a machine. Platelet component of the blood is separated, concentrated and then injected in the patient. When Platelet Rich Plasma is injected into the damaged area it stimulates the tendon, ligament or muscle with a high concentration of growth factors that triggers the healing cascade. As a result new tissue begins to develop. As this tissue matures it begins to shrink causing the tightening and strengthening of the tendons, ligaments and muscle of the damaged area. Patients suffering from Arm, Shoulder, Leg or Hip Pain might benefit from this procedure.
Transcutaneous electrical nerve stimulation (TENS) involves wearing a battery-powered device consisting of electrodes placed on the skin over the painful area that generate electrical impulses designed to block incoming pain signals from the peripheral nerves. The theory is that stimulating the nervous system can modify the perception of pain. Early studies of TENS suggested that it elevated levels of endorphins, the body’s natural pain-numbing chemicals. More recent studies, however, have produced mixed results on its effectiveness for providing relief from low back pain.